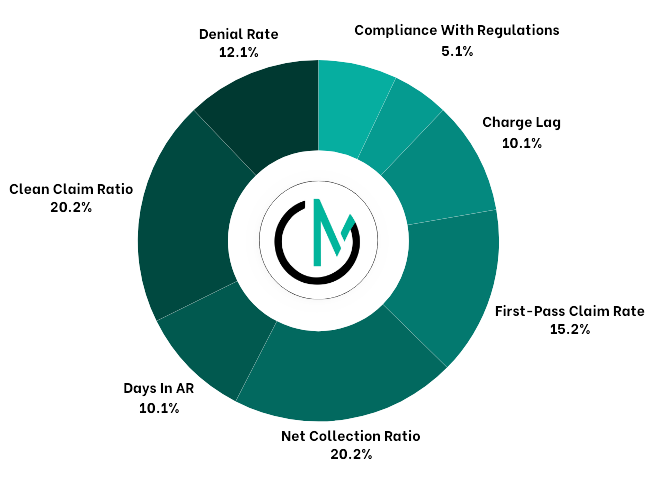
ONE
24/7 Access to Cutting-Edge Technology
Advanced billing technology and coding expertise provide seamless support for operations, customizing billing and revenue cycle management for large practices. Outsourcing billing gives access to this expertise without incurring additional software or hardware costs.